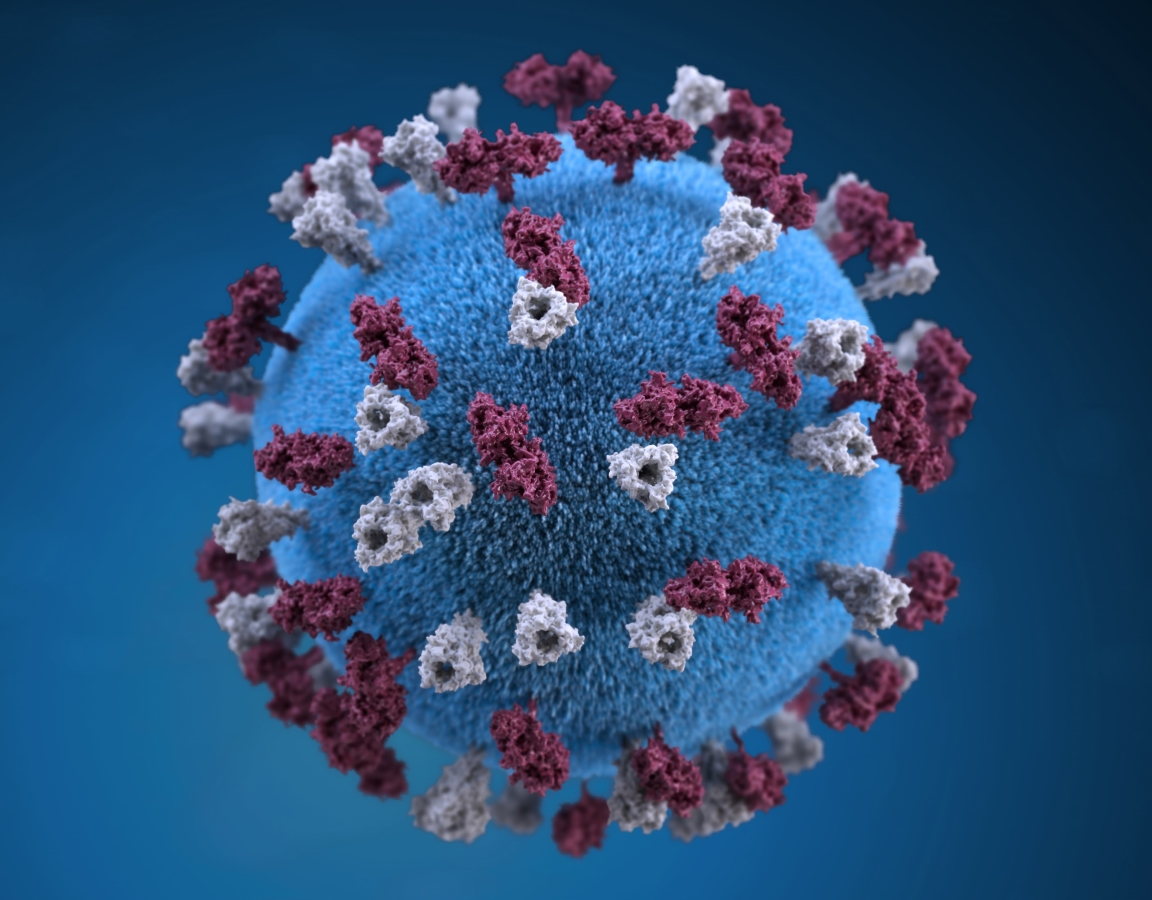
Shelter-in-place orders and concerns over exposure to COVID-19 have many Americans second-guessing in-person visits with their doctor. Instead, people are using telemedicine in unprecedented numbers, getting the healthcare they need without leaving the house.
Telehealth visits increased 50% in March after President Trump declared a national state of emergency and his administration encouraged doctors and patients to utilize them.
Employers are also promoting the use of virtual care. In a recent survey of employers’ responses to the pandemic, 86% of respondents said they are promoting the use of telemedicine, nurse lines or virtual healthcare visits to their employees, and 58% are increasing access to telebehavioral health with another 14% planning to do so.
Analysts predict that, in 2020, telehealth visits will exceed 900 million for coronavirus-related concerns and 200 million for general medical care. The forecast was initially 36 million visits this year. Telemedicine has been around for decades, steadily expanding and gaining popularity. However, this recent uptick in demand has providers scrambling to adapt.
If it isn’t on your radar, here are 5 reasons to use telemedicine as a convenient option while social distancing. You can interface with board-certified healthcare professionals from the comfort of home, or most anywhere else, often 24/7.
The scope of services that can be delivered this way may surprise you. As we adjust to life during the coronavirus, virtual healthcare can play a role in screening for the virus itself, treating medical issues and receiving mental health therapy.
1. COVID-19 Screening
Telemedicine is playing a big role in patient screening for COVID-19. Not everyone needs a diagnostic test, according to the CDC. As such, remote screenings help triage patients at a time when healthcare facilities are trying to reduce exposures and ensure personal protective equipment is used effectively.
That means you’re likely to talk with a healthcare provider on the phone or through a virtual appointment if you are experiencing symptoms of the coronavirus. This will help determine your next steps (e.g., getting tested, staying home to recover unless your condition worsens).
To learn how to get screened for COVID-19, contact your healthcare provider or state or local health department, or visit their respective websites. If you are having a medical emergency, call 911 — emergency warning signs for COVID-19 include trouble breathing and persistent pain or pressure in the chest, to name a few.
2. Medical Appointments Unrelated to the Coronavirus
While some states have encouraged and continue to encourage delaying elective medical procedures, that doesn’t mean you can’t get medical attention unless you have COVID-19 symptoms or an emergency.
Telemedicine without the waiting room makes it possible to be safely seen by a healthcare professional while you shelter in place — no worries about staying 6 feet apart, wearing a mask or being exposed to the coronavirus (or anything else) — and experts are encouraging people to take advantage of it.
Conditions that may be diagnosed and treated through a telemedicine consultation include, but are not limited to, rashes, ear and eye infections, allergies, sinus infections and urinary tract infections. Providers can also prescribe and write refills for medications during telehealth appointments. Even dentists have been using teledentistry to assist patients in acute situations and keep them away from the emergency room.
When telemedicine isn’t an option
Of course, not everything can be treated from a distance. Your telemedicine appointment may determine its necessary to schedule an in-person visit with your healthcare provider. Depending on the urgency, you may not be able to wait until social distancing precautions ease.
It also needs to be said that you should call 911 or go to the emergency room if you’re having a medical emergency. Unfortunately, fear of catching the coronavirus seems to be keeping people away from emergency rooms and preventing them from calling 911 right now, which concerns healthcare providers who wonder if they will see a future increase in bad outcomes due because people delayed care.
Medical professionals want you to know that hospitals and clinics are taking precautions to keep people as safe as possible and that a medical crisis can turn deadly if you delay going to the ER or calling 911.
3. Mental Health Therapy
It may be a virus, but COVID-19 is having a significant impact on mental health. Job and income loss, shifting routines and family dynamics, social isolation, and staying healthy are just some of the stresses caused by this pandemic. The need for support is high.
Calls to the Disaster Distress Helpline increased 891% in March 2020 over March 2019. In April, 56% of U.S. adults reported that the coronavirus had caused at least one negative effect on their mental health and well being; 64% of frontline healthcare workers and their families reported the same.
Whether you’re a new or existing patient, telemedicine makes it possible to remotely seek or continue care. You may be able to work with a therapist by phone or online.
Fortunately, access to virtual therapy visits is expanding. Behavioral health providers, including psychologists, psychiatrists, licensed clinical social workers and licensed practicing counselors, been working to quickly get their services online. In the past, regulation and reimbursement have been barriers; however, some federal and state restrictions have been temporarily eased to allow for broader availability.
As for patients, cost is often a barrier to help. At this time when many are struggling, some insurers are waiving copays to make mental health treatment more accessible. There are also many no-cost resources available, some of which are identified in the list below. But overall, telemedicine is a healthcare money saver.
How to connect with a therapist from home
If you need help finding a mental health professional, here are some ways to get started:
- If you are insured, contact your insurance company or search your plan’s online directory to find in-network providers who are accepting new patients. You may need to contact those providers to see if they offer a teletherapy option.
- If you have telemedicine benefits that include teletherapy, you can be connected through your telemedicine provider.
- Search for a Federally Qualified Health Center near you. FQHCs provide reduced cost or free care dependent on need, and they can offer telehealth counseling at this time.
Some additional ways to find and access remote help include the following:
- Visit Postpartum Support International for an extensive list of resources available to families and parents.
- The national crisis text line (text CRISIS to 741741) is available 24/7 and someone will respond to you within minutes.
- Make a free phone appointment with the COVID-19 Emotional Support Hotline; call 844-863-9314
- The National Alliance on Mental Illness has put together an extensive COVID-19 Resource and Information Guide. You can also call the NAMI HelpLine at 800-950-6264.
- The Substance Abuse and Mental Health Services Administration has also put together a list of resources and information to help those facing challenges amid the COVID-19 pandemic.
Call 911 if you’re in crisis.
How Telemedicine Works
Before you schedule a telemedicine appointment, you will need to determine where to do so and how you will pay for it. If possible, research this ahead of time so you have everything in place (e.g., account set up) when you need care.
Your existing healthcare provider may offer virtual appointments, which may or may not be covered by your insurance. Otherwise, you will use the telemedicine service your insurance plan includes.
Depending on who provides your telehealth services, your consultation may take place by phone or video. Video appointments may take place through an app or web portal. The exact process and format varies. Your healthcare or telemedicine provider will provide guidance on how to get started.
Where to Get Telemedicine Benefits
An increasing number of health insurance plans now include benefits for telemedicine. Check with your insurer to find out if and how your policy covers it (e.g., coinsurance, flat fee). For example, plans available through Pivot Health include unlimited telemedicine doctor consultations at no additional cost.
If your short-term medical, individual medical or job-based health insurance plan doesn’t include telemedicine, you can still access telemedicine consultations through a virtual healthcare provider for a fee.
What if you are a Medicaid or Medicare beneficiary? The Trump administration is temporarily expanding telemedicine rules for Medicaid and Medicare. A broader range of services will be available through audio and video communication — these services are not limited to coronavirus-related conditions. As with other forms of health coverage, check with your Medicare or Medicaid plan with questions about telemedicine before you seek care.
As for teledentistry, it may or may not be covered by your health insurance — some insurances have been covering it during the COVID-19 crisis. Contact your health or dental insurer to confirm benefits.
The Future of Virtual Healthcare
COVID-19 will continue to transform the healthcare landscape, and mainstream adoption of telemedicine will surely be among the lasting effects. Yet, experts point out that there will be challenges along the way such as meeting government standards for privacy and improving access to affordable, high-quality broadband.
The pandemic may help force the issue of telemedicine improvements nationwide as state and federal governments, insurers, healthcare providers and others involved with the healthcare system work to catch up with consumer demand.



 877-246-0106
877-246-0106

